IN VITRO FERTILIZATION (IVF)
IN VITRO FERTILIZATION (IVF)
WHAT IS IN VITRO FERTILIZATION (IVF)?
In Vitro Fertilization (IVF), in essence, consists of putting the eggs and sperm into contact in the laboratory to achieve the formation of embryos that will be transferred (1-2) into the woman’s uterus for implantation. The time the embryos are kept in the laboratory depends on their quantity and quality. Likewise, IVF will have different variables according to the origin of the eggs and sperm, since these can be their own or from a donor. IVF can also be accompanied by other techniques in the laboratory that enrich it, such as: MACS, Fertility, embryo freezing, preimplantation diagnosis, etc.
IN WHAT CASES IS IT INDICATED?
- Failure of other techniques, such as various failed Artificial Inseminations (AI)
- Moderate and severe male factor (when the REM test recovers less than 5 million spermatozoa with good motility)
- Advanced maternal age (> 38-40 years)
- Tubal factor (when the fallopian tubes are partially or totally blocked)
- Advanced grade III and IV endometriosis.
- Ovarian dysfunction.
- Infertility (repeat abortions)
- Sterility of unknown origin
- Long-term sterility
- Hereditary genetic diseases
- Risk of transmission of infectious diseases to offspring.
THE STAGES OF THE IVF PROCESS

THE STAGES OF THE IVF PROCESS


FIRST VISIT
As with all treatments that take place at Embriogyn, the first step is to make a first visit so that a good case study can be indicated. During this visit, an exhaustive study of the medical and reproductive history will be carried out with one of our fertility gynecologists. Therefore, it is important to bring, if you have it, all the information related to the reproductive history prior to the consultation. In addition to a complete gynaecological study, a study of the semen will be indicated, in the case of the couple, in order to make the most detailed and personalised diagnosis possible.
OVARIAN STIMULATION
One of the reasons why the probability of gestation is increased through IVF is because we have more eggs in the same cycle, since the process is optimized, generating more embryos that we can select better to transfer to the mother’s womb and give rise to a healthy baby at home with more success.
In order to have more than one egg, which is what would be normal in a natural menstrual cycle, we proceed to administer hormones that act on the ovary. The doses used should be individualized according to various parameters, such as body mass index (BMI), age of the woman, first phase hormonal determinations, morphology of the ovaries (number of preantral follicles), response to stimulation in previous cycles if there has been and the experience of our professionals.
Careful control of ovarian stimulation requires several ultrasound controls (4 or 5) to monitor well the response achieved in each case. The stimulation process usually lasts between 8 and 12 days. Once it has been checked that the hormone levels and the number and size of the follicles are as desired, a final medication is administered to trigger the maturation of the eggs by means of a hormone called human chorionic hormone (HCG).


EGG RETRIEVAL
The extraction of the eggs, or follicular puncture, is carried out in the Centre’s own minor outpatient surgery theatre, under sedation, by means of ultrasound control, transvaginally, some 36 hours after the administration of the HCG. The extraction of the eggs is carried out by means of the puncture of the mature follicles and subsequent aspiration of the follicular fluid where the egg should be found. The person responsible for this process is the same gynaecologist specialised in fertility who performs the technique.
The average duration of this intervention is about 15-20 minutes and is performed under anesthesia (deep sedation) to avoid discomfort to the patient and controlled by one of the anesthesiologists of the Center who will ensure the control of the patient at all times.
The woman’s recovery is rapid, as after 1 or 2 hours, she is discharged from the hospital.
At the same time as the operation is being carried out in the operating theatre, the team of biologists is looking for the extracted eggs to be able to store them in incubators and continue the process of in vitro fertilization. This is why, by the time the patient wakes up, she can already know the number of eggs that have been obtained.
IVF LABORATORY
Identification and collection of the eggs
The follicular liquids obtained in the puncture are taken to the IVF Laboratory where all the eggs are located and collected at the same time as the gynaecologist is carrying out the extraction of the eggs. These are placed on plates with a suitable culture medium, duly identified and numbered, inside the incubator. This is one of the entry points for the control of the traceability of the eggs which is controlled by the Witness security system. The incubators keep them in a suitable environment in terms of temperature, humidity, proportion and purity of gases.
Semen preparation
In the Andrology Laboratory, the sperm sample will be processed with the most appropriate sperm training technique according to the quality of the semen. These techniques allow us to select and isolate the spermatozoa with the best motility, morphology and/or lower DNA fragmentation rate. This is another entry point for the Witness security system’s sperm traceability control.
Fertilization technique
The next step is to proceed with the fertilization of the eggs and sperm. There are mainly two methods to facilitate fertilization:
Conventional Fertilization: is the procedure in which the eggs, which are still within the clusters (group of cells that surround the egg), are placed in the same medium with the previously treated spermatozoa, with the intention of carrying out fertilization spontaneously. To perform this technique, a minimum concentration of spermatozoa with good mobility of 100,000 spermatozoa per milliliter and per ovum is required.
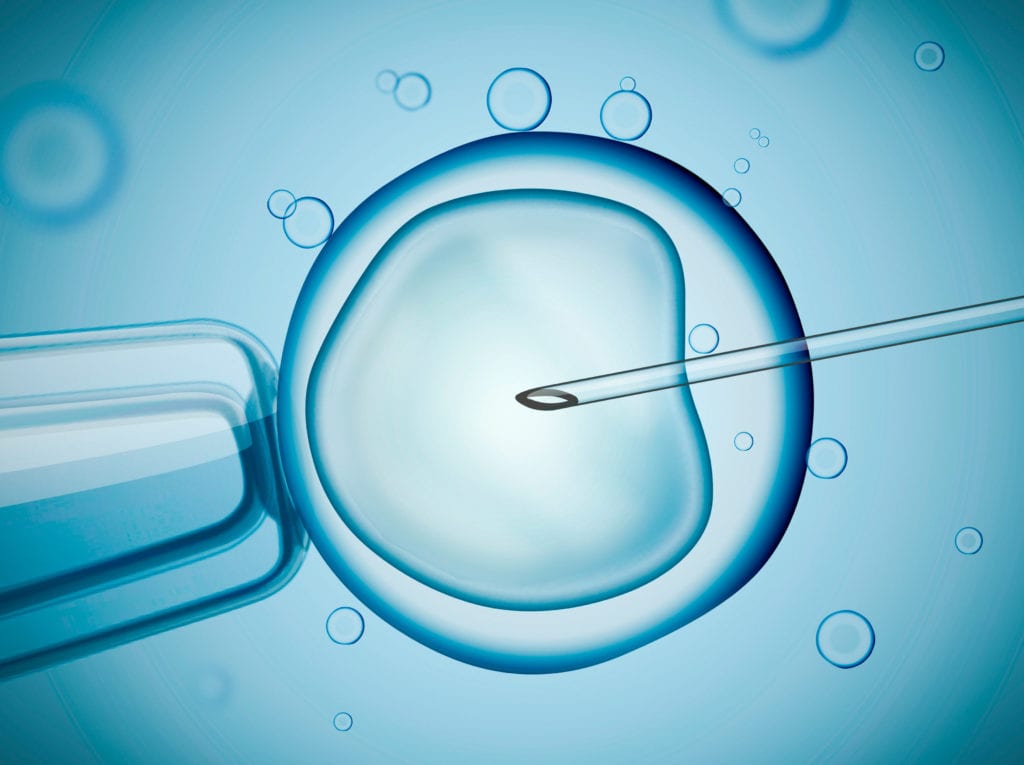
ICSI (Intra Citoplasmatic Sperm Injection): consists of directly introducing a spermatozoon into a mature egg by means of micromanipulation. Embriogyn’s teams, together with the high level of training and experience of our embryologists, allow us to achieve very good fertilization rates, which are around 75% in most cases. Thanks to this technique, only one motile spermatozoon is needed for each mature egg. Therefore, this technique can be applied to very low quality sperm samples, even in Testicular Biopsy.
Assessment of fertilization
The validation that the fertilization has taken place correctly is carried out after 16-20 h post ICSI or Conventional Fertilization. For fertilization to take place, it is a sine qua non condition that the embryo has its own structures, which are two pronuclei, one coming from the egg and the other from the sperm. Any variable or the non-presence of these structures means that the fertilization has not been correct and therefore we discard these eggs to continue the process.
Embryo culture, the EMBRYOSCOPE
The Embryoscope is a time-lapse culture system that provides continuous images of the embryos. Since 2011, Embriogyn joins the revolution in reproductive medicine with the application of this technology to all patients of the center, which has allowed us to improve gestation rates by about 15 -20%.
The fertilized eggs, now embryos, are kept in culture in the Embryoscope incubator for 3-6 days before being placed back into the mother’s womb. This embryo culture allows the development of the embryos in vitro and allows us to continuously evaluate the evolution of each one of them and to have the necessary information to choose the best ones to be transferred to the maternal uterus. This information provided by the Embryoscope is shared with our patients allowing each one to see their own embryos, thus providing confidence and transparency in the whole process being carried out in the In Vitro Fertilization laboratory, as well as a greater degree of knowledge and understanding of the evolution of the embryos.

EMBRYO TRANSFER
The best time to return the embryos to the mother’s womb is decided in each individual case. Depending on many factors such as the characteristics of the embryos and the medical and reproductive history of the couple, the embryologist advises the most appropriate time of transfer (normally on the third or fifth day of embryonic development).
The transfer is a simple and painless procedure, which normally does not require anesthesia. With the help of a very thin catheter, the embryos are deposited in the fundus of the uterus. This process is controlled by abdominal ultrasound.
At present, 1 or 2 embryos are transferred, in consensus with the couple and the medical advice that evaluates the individual history of each case in order to obtain the highest probability of gestation while minimizing the risk of multiple pregnancy.
On some occasions, the transfer of fresh embryos may be discouraged for various reasons. Therefore, all the embryos obtained in this treatment are frozen for later transfer in a cryotransfer process.
VITRIFICATION OF THE REMAINING EMBRYOS
Once the transfer of the selected embryos has been carried out, the remaining embryos of good quality are frozen in order to preserve their potential for later transfer.
The technique used for freezing the embryos is vitrification, which gives very high survival rates and the same probability of pregnancy as fresh embryos.
Embryo freezing becomes a very good fertility preservation system, although one must be very strict to freeze only those embryos that really have fertile potential to give real expectations to parents who later wish to make use of their frozen embryos.


GESTATION TEST AND ULTRASOUND
Once the technique has been completed, you will rest for a few minutes, we will give you the instructions to follow and we will set a date to do the pregnancy test with the first urine in the morning approximately 14 days after the extraction of the eggs. During this period, we recommend living a completely normal life, maintaining your usual routines and avoiding only high intensity efforts. We will also give you some guidelines to reduce the stress of waiting and transform it into a positive attitude to live it as naturally as possible.
Three weeks after the positive result, an ultrasound scan will be carried out to check the viability of the pregnancy. This ultrasound scan is performed in the 6-7 week of pregnancy, where the gestational sac and yolk sac of the embryo can be seen already with a heartbeat. From then on this gestation is like any other and requires the normal follow-up and controls of a pregnancy and together we can celebrate the success!
Women < 35 years
Between 35 and 38 years old
Between 39 and 42 years old
Women > 42 years
WHAT DOES TREATMENT INCLUDE?
- Hormone tests during the cycle
- Medical visits and hormonal stimulation controls
- Follicular puncture and anesthesia
- IVF lab processes
- Andrology lab processes
- ICSI (Intracytoplasmic Sperm Injection)/IVF
- Embryo culture with Embryoscope technology
- Embryo Transfer
-
B-HCG pregnancy test
- Ultrasound to verify pregnancy
- Witness system of security and traceability of biological samples
PRICE OF TREATMENT: 4590€
MAKE AN APPOINTMENT
It’s quite simple. All you have to do is contact Embriogyn and make an appointment with our specialists at the time that suits you best. In case you can’t come in person to the clinic, visits can also be arranged via Skype.
